Hours: Thurs-Mon, noon-6 pm

If you’ve ever browsed cat adoption profiles and come across the phrase “feline herpes positive,” you might hesitate at first. It sounds intimidating—but it doesn’t have to be. With a bit of knowledge and some extra loving care, cats with FHV-1 can live happy and healthy lives just like any other cat. In this article, you’ll learn what feline herpes is, what can trigger flare-ups, and how simple, informed care can make adopting an FHV-1 cat a deeply rewarding experience.
Because of its latency and potential reactivation, FHV‑1 is often misinterpreted as a chronic disease—but it behaves more like a “flareable” virus than a constantly debilitating one.
Feline herpesvirus type 1 (FHV‑1), also called feline viral rhinotracheitis (FVR), is one of the most common viral infections in cats. Any cat can contract FHV-1, but younger cats are most often affected. FHV-1 can be spread through saliva as well as nasal and eye discharge, either directly from the cat or from a contaminated object like a toy or food dish. After initial exposure, the virus typically causes an upper respiratory and ocular infection (sneezing, nasal/eye discharge, conjunctivitis) lasting around 10–20 days in mild cases.
Even once the acute symptoms have resolved, the virus remains in a dormant state in nerve tissues for the cat’s life. The virus is most likely to reactivate if the cat experiences stress or an immune system challenge. When it reactivates, it causes a flare-up. Many cats experience very mild or even subclinical symptoms when a flare-up occurs.
FHV-1 vs. FIV vs. FeLV
It’s easy to confuse FHV‑1 with other feline viruses like FIV (feline immunodeficiency virus) or FeLV (feline leukemia virus), but they’re quite different. FHV‑1 is a respiratory virus that causes flare-ups like sneezing and eye discharge, but doesn’t impact a cat’s immune system the way the other two do. FIV is an immune-compromising virus primarily spread through deep bite wounds, while FeLV is a retrovirus that can suppress immune function and is more easily spread through prolonged close contact like grooming or shared dishes. Each virus has its realities, but none are an automatic disqualifier for a loving, quality life.
Myth 1: “Having FHV-1 means the cat will have a low quality of life that’s filled with constant illness and discomfort.”
Reality: Most cats recover from initial infection and go on to lead essentially normal lives. While younger kittens, immunocompromised cats, or those with other illnesses might experience a more severe disease, serious outcomes are relatively rare in otherwise healthy cats.
Myth 2: “A cat with FHV-1 will always be symptomatic.”
Reality: Many cats are asymptomatic carriers most of the time, with flare-ups only under stress (e.g. moving, travel, other illness). In fact, viral shedding (when the cat is contagious) is much more likely during active episodes; in dormancy, shedding is minimal or absent.
Myth 3: “Herpes in cats is like herpes in people and can spread to humans or dogs.”
Reality: FHV‑1 is species-specific; humans and dogs cannot contract feline herpes.
Myth 4: “You can cure FHV-1 completely.”
Reality: There is no cure for herpes in cats. The goal is managing symptoms, reducing flare frequency and severity, and supporting the cat’s overall health through good nutrition and enrichment.
Myth 5: “You can prevent FHV-1 completely.”
Reality: One of the core vaccines recommended for kittens and adult cats by the Feline Veterinary Medical Association is the FHV-1 vaccine. While this vaccine doesn’t completely eliminate the chances of the cat contracting FHV-1, it is highly effective at preventing severe illness, including symptom severity and duration, and it also helps limit the cat’s viral shedding and how contagious it is to other cats. This vaccine is often administered as part of a combination vaccine called FVRCP, which protects against Feline Viral Rhinotracheitis, Calicivirus, and Panleukopenia. All cats at Cat Care Society are given the FVRCP vaccine according to the recommended schedule.
As you can see, the reality is that cats with FHV-1 can still live long, happy lives with proper care, love, and a stable environment that supports their health and comfort.
If a shelter informs you that a cat you’re interested in adopting has FHV-1, keep the following considerations and tips in mind to help your future feline friend thrive:
At CCS, if a cat is suspected of having feline herpes, it will be noted in their medical records along with information about the virus. It’s also important to understand if the cat has any other co-existing conditions, like upper respiratory illness or eye concerns, that might complicate flare management. Understanding the individual cat’s history gives you a more accurate sense of what to expect so you can be prepared. You should also share this information with your veterinarian so they can create a treatment and management plan. In most cases, FHV-1 symptoms are non-life threatening and the cat will respond well to general supportive care.
Be aware of the respiratory and ocular signs of a flare-up, such as sneezing, watery eyes, discharge, and corneal irritation or ulcers, especially in times of stress. During those times, vet support (antivirals, topical ocular medication, secondary infection treatment) plus extra care at home can often resolve symptoms.
Stress is one of the strongest triggers for viral reactivation. Strategies to help minimize stress include:
Even when asymptomatic, certain practices, in addition to stress reduction, can reduce flare risk and flare severity:
Many potential adopters hesitate when they see an FHV-1–positive cat, but choosing to adopt one and offering them a loving home can be truly life-changing—for both of you. Here at CCS, we’ve received many heartwarming updates from adopters whose herpes-positive cats are thriving, underscoring that with care and compassion these cats can live long, joyful lives. If you’d like more information on FHV-1, including details on how the virus works and common treatment regiments, check out this great article by VCA Animal Hospitals.
About the Author: Beth Dokolasa is a volunteer for Cat Care Society and serves on the Board of Directors. She is an instructional developer for Natural Grocers and lives in Indian Hills, Colo., with her husband, daughter, and two cats, Techno and Digit.

There are more cat food options than ever before, which is great for picky eaters and for cats with special dietary needs, but for a cat owner, navigating the cat food aisle can feel overwhelming. The good news is that with so many options available, even if you’re on a budget, you can still provide your cat with healthy and tasty food. In this article, we will discuss what to look for on the label, pros and cons of various cat food forms, and much more!
The best way to begin filtering through all the cat food options is by knowing what to avoid and what to look for on the product’s label.
What to Avoid:
Food Fact: Terms like “premium,” “gourmet,” “holistic,” “no fillers,” and “human-grade” aren’t legally regulated and don’t guarantee higher-quality ingredients. While foods with these labels aren’t always bad choices, it’s important not to rely solely on these words when choosing a cat food, as they have no official definitions or standards.
What to Look For:
If you’re still having trouble making a decision, you can always ask your veterinarian for suggestions. If your cat needs a specific prescription diet, always follow your veterinarian’s guidance. Also, if you’re adopting a cat, ask the shelter what food the cat has been eating and what they’d recommend. At Cat Care Society, we’re a big fan of Hill’s!
Food Fact: The terms “complete” and “balanced” are defined by AAFCO and are regulated by the Food and Drug Administration (FDA). You can feel confident that when you see “complete” on a cat food, it contains all the required nutrients for a cat. “Balanced” means it contains all the nutrients and they are in the ideal proportions.
Below are the most common forms of cat food. There’s no single perfect choice for every cat, so you may need to experiment to find what best suits your cat’s tastes and your lifestyle.
Dry Kibble: Shelf-stable, cost-effective, and convenient to measure and store, dry kibble is often a significant part of a cat’s diet. There are many options available—from formulas with specific textures to help reduce plaque and tartar, to those fortified with vitamins, minerals, and other specialty ingredients aimed at specific health goals.
Canned/wet food: Containing 70–80% moisture, canned/wet food can support kidney and urinary tract health, especially in cats that don’t drink much water. Wet food is usually very popular with cats, and sometimes essential for cats with dental issues. Some kitties may have a preference between pâté, chunks in gravy, flakes, shredded, etc., so try single cans first before buying in bulk!
Fresh/refrigerated food: This option involves fresh, but cooked, foods that are often steamed to preserve nutrients while reducing harmful pathogens. Safe food handling is still essential to ensure the food remains safe to eat throughout storage and consumption, and be sure to look for complete and balanced options.
Raw/freeze-dried raw food: The goal of commercial raw/freeze-dried raw food is to provide high-quality protein and mimic a cat’s natural prey-based diet. However, most raw cat food products are not complete and balanced, and they also carry a much greater risk of foodborne illness in your pet and in the people living in the household. Additionally, it is not recommended to feed your cat raw meat purchased at a traditional grocery store as it carries a greater risk of illness due to harmful bacteria like Salmonella and E. coli. In recent years, feeding cats raw and freeze-dried cat food has also come with an increased risk of bird flu transmission. The Food and Drug Administration (FDA) has some great research and guidance on raw pet food diets.
Many cats enjoy a combination of foods. This could look like mixing dry food in with a wet pâté at meal time or serving them separately, such as wet food in the morning and dry kibble for their evening meal. The most important thing is to choose foods with a nutritional adequacy statement on the label, which confirms they are complete and balanced and meet AAFCO nutrition standards.
One thing is for sure: cats need meat. Cats are obligate carnivores, which means they need to eat meat to stay healthy. In general, cats do best eating a diet with high amounts of protein, moderate amounts of fat, and minimal amounts of carbohydrates. Check out our blog post that goes into more detail on why cats need to eat meat to learn more!
Food Fact: Each cat is unique, and their dietary needs are unique, as well. General recommendations given in our blog or on the food products you purchase may not be the best fit for your cat. We always recommend consulting your veterinarian when deciding on the best types and amount of food to feed your cat daily.
Whatever you call them, choosy cats can make it difficult to find that balance of nutritious, delicious, and budget-friendly. A good place to start is by switching up the consistency and texture, because a cat’s senses are especially sensitive to it. From having a jaw designed for shearing meat and crunching bones to having highly sensitive whiskers and lips, they notice the subtle differences in food shape, size, and feel. For example, certain cats may love shredded wet food in gravy but stick up their noses to chunks in gravy. Below are some ideas to satisfy your feline foodie.
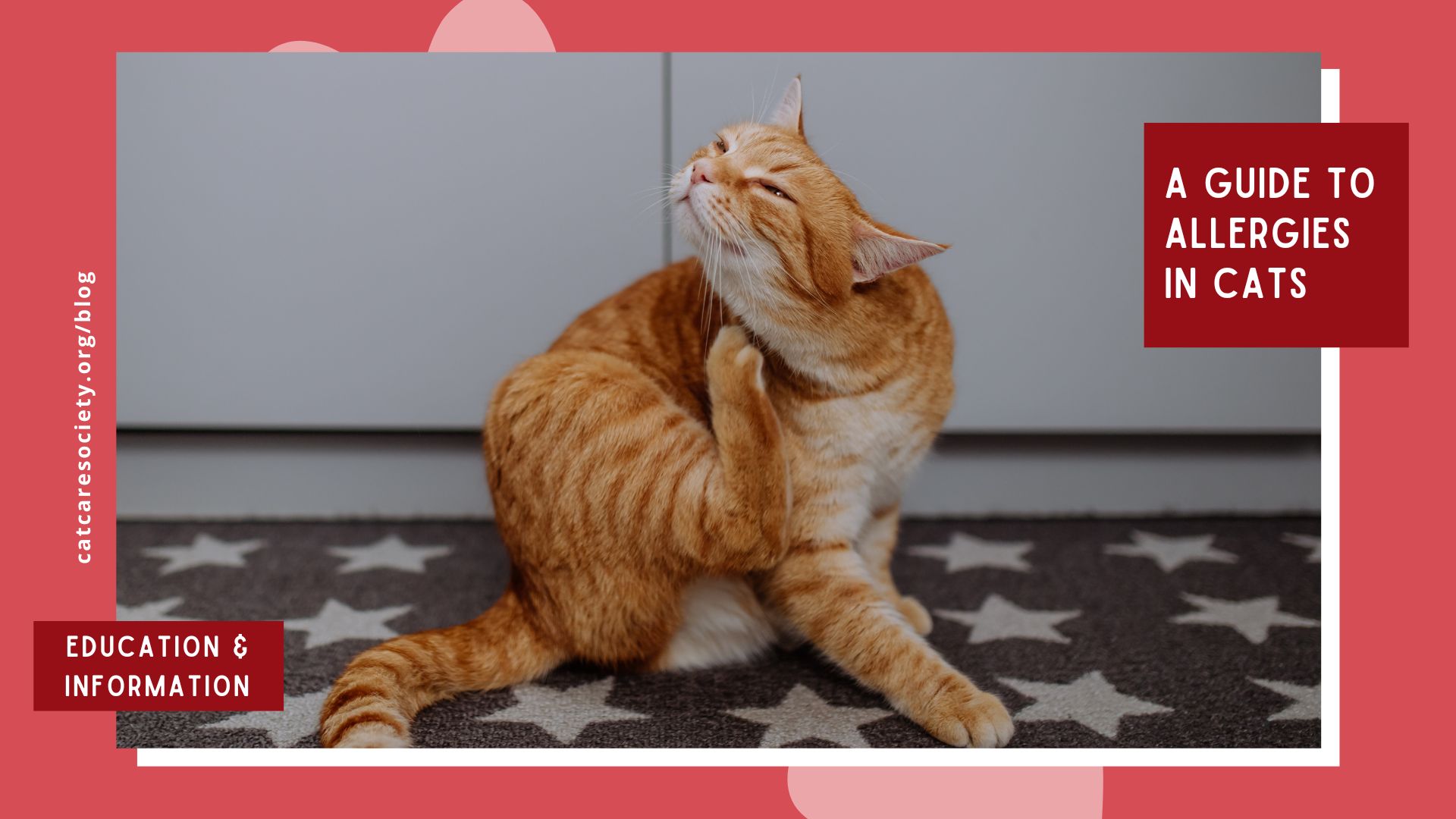
When to Visit a Vet: If you notice a sudden change in your cat’s food preferences, it’s a good idea to visit your veterinarian to rule out any new health conditions or dental issues. Additionally, if you notice your cat excessively scratching, licking, or biting their skin, it may indicate that they have a food allergy.
By paying attention to the label and choosing foods that meet AAFCO standards for your cat’s life stage and health needs, you can ensure your cat gets the nutrition they need. Remember that different forms of cat food—dry kibble, wet/canned, raw/freeze-dried, or fresh/refrigerated—each have their benefits, and many cats thrive on a mix. For picky eaters, experimenting with texture, temperature, and food enhancers can make mealtime more enjoyable.
Donate you extra cat food to CCS! If you have leftover cat food that your cat doesn’t enjoy or food you simply no longer need, consider sharing it with other cats. CCS gladly accepts any non-refrigerated, unexpired cat food or treats—wet or dry, new or partially used (in their original packaging). Simply bring your donations during shelter hours and leave them in the designated donation area in the lobby.
About the Author: Beth Dokolasa is a volunteer for Cat Care Society and serves on the Board of Directors. She is an instructional developer for Natural Grocers and lives in Indian Hills, Colo., with her husband, daughter, and two cats, Techno and Digit.

Cats are often known for being picky eaters—whether it’s an aversion to certain kibble shapes, a preference for pâté over chunks in gravy, or a liking for food served slightly warmed. For cat owners, finding a food that their cat enjoys while still meeting nutrition needs can be a real challenge. However, one thing remains certain: cats are obligate carnivores and need to eat meat.
An obligate carnivore is an animal that must eat meat to survive because its body is biologically adapted to derive essential nutrients solely from animal-based sources. Cats evolved as hunters that consume prey containing high amounts of protein, moderate amounts of fat, and minimal amounts of carbohydrates, and they still typically do best consuming those proportions today. Just like humans, cats also require certain amounts of micronutrients, like vitamins, minerals, and amino acids to thrive.
Cats require many kinds of micronutrients from a variety of sources. Below are some of the key nutrients that are either exclusively found in meat or for which meat is the best source.
Without adequate intake of these vital nutrients, cats can experience deficiency symptoms and even irreversible damage to their health, so it’s important to provide them with a complete and balanced diet that reflects their biological need for meat-based nutrition.
Food Allergy Note: Even though cats need meat, they can still develop allergies to certain kinds of meat. The most common meat allergens for cats are beef, chicken, and fish. If you regularly feed these to your cat and notice them scratching, licking, or chewing themselves more than usual, they may have a meat allergy. Your cat’s veterinarian may recommend an elimination diet trial where you avoid the foods they regularly eat for a designated time to see if the symptoms improve. Alternative meat protein like rabbit, duck, and venison are often good options for cats with known meat allergies.
If you’re starting to think this is all leading to a time-consuming recommendation for homemade, all-meat meals—don’t worry. Regardless of quality, feeding your cat only prepared muscle meat (such as chicken breast or ground turkey) can actually lead to essential nutrient deficiencies! Cats need a variety of nutrients found in organ meat and animal fat, too. For balanced and complete nutrition, cats typically do best consuming commercially balanced raw and cooked food.
Look for products that contain a nutritional adequacy statement on the label. This indicates that the food meets the nutritional standards set by the Association of American Feed Control Officials (AAFCO), a nonprofit that establishes nutritional standards for pet foods. Cat Care Society is a proud partner of Hill’s Food, Shelter & Love program, and we feed Hill’s to our shelter cats. Hill’s recipes meet AAFCO nutrition standards, so our cats get the complete and balanced nutrition they need. (Note: AAFCO does not directly test or certify pet foods. Pet food companies use third-party testing agencies to analyze their foods according to AAFCO guidelines.)
Supplemental homemade meals can often be included as a part of your cat’s healthy diet, provided that it’s approved by the cat’s veterinarian, safely prepared, and does not include any ingredients harmful to cats, such as garlic, onions, raw eggs, and excess sodium. Additionally, do not feed your cat raw meat. While cats eat raw meat in the wild, feeding them raw meat purchased at a traditional grocery store can cause illness due to harmful bacteria like Salmonella and E. coli.
Understanding your cat’s biological need for meat is essential to supporting their lifelong health and well-being. As obligate carnivores, cats rely on meat not just for protein, but for critical nutrients like taurine, arachidonic acid, and essential vitamins that they cannot make on their own. By choosing high-quality commercial foods that meet AAFCO standards and consulting with your veterinarian, you can feel confident that you’re giving your cat the nourishment they need to thrive.
About the Author: Beth Dokolasa is a volunteer for Cat Care Society and serves on the Board of Directors. She is an instructional developer for Natural Grocers and lives in Indian Hills, Colo., with her husband, daughter, and two cats, Techno and Digit.

If you love cats, you may have heard the term “kitten season” before—but what exactly does it mean? Kitten season is the time of year when shelters and rescues typically receive an influx of newborn kitten litters as well as their mothers. This surge in cats can create challenges for pet shelters, but with the right knowledge and support, everyone can play a part in helping shelters, ensuring the well-being of the cats, and finding them a loving home.
Kitten season typically occurs from early spring through late fall, with a peak in the warmer months. During this time, unspayed female cats go into heat more frequently and have the potential to give birth to multiple litters, with an average of 4-6 kittens born per litter. This can really add up! Many of these kittens are born outdoors to feral or stray cats and end up in shelters or on the streets.
While kittens are undeniably adorable, the large number arriving at shelters during kitten season creates a high demand for resources like medical care, food, and space. In Colorado, kittens cannot be adopted until they are two months old so shelters are providing lots of long term care for them! Shelters and rescue organizations work tirelessly to care for these kittens and their mothers, but they often face challenges like overcrowding and foster home shortages.
Foster homes help address space shortages but they also play a crucial role in keeping all cats healthy. Kittens don’t yet have a fully developed immune system or GI tract making them more vulnerable to catching and spreading illnesses, which can further overwhelm the shelter and impact other cats. Kittens do not begin to receive illness preventing vaccines until they are at least four weeks of age. Additionally, kittens require frequent monitoring, socialization, and specialized care, which can be challenging for shelters managing many animals at once. Foster caregivers help by providing individualized attention, ensuring kittens receive the care they need to grow strong and healthy before adoption.
To reduce the number of kittens in shelters and ease the ongoing pressure on resources, shelters also focus on spaying mother cats, preventing future litters. This helps break the cycle of overcrowding and ensures that shelters can better meet the needs of all the cats in their care. With community support—through fostering, adoption, and other forms of assistance—we can give every kitten the best chance at a healthy, happy future.
There are many ways you can make a difference during kitten season. Whether you’re able to adopt, foster, volunteer, or support from afar, every effort counts. Here are some suggestions:

Many shelters and rescues rely on foster homes to care for young kittens
who are too small to be adopted. These kittens need a safe and loving environment where they can grow, socialize, and receive proper medical care. Fostering is a rewarding experience and saves countless lives. Learn more about being a foster with Cat Care Society and apply online.
Preventing unwanted litters starts with responsible pet ownership. Ensure your own cats are spayed or neutered, and encourage friends and family to do the same. We have a resource list of lost-cost clinics that can help make this more accessible. Encourage your friends and family to read more about the benefits of spaying and neutering your cats in one of our other blog posts.
If you’ve been thinking about welcoming a cat into your family, kitten season is an ideal time to adopt. Shelters are overflowing with kittens and adult cats looking for homes. We also suggest adopting two kittens at the same time so they can continue practicing great behavior habits! By adopting, you’re not only giving a cat a second chance but also freeing up space in shelters for other animals in need. Check out our cats available for adoption!
Cat Care Society has a robust in-house cat socialization and enrichment program, and we also have many great resources to help you bond with your new kitty once it’s home and set up an environment where your cat can play, express their natural behaviors, and thrive!
One of the most effective ways to reduce the number of kittens born on the streets is through Trap-Neuter-Return (TNR). This humane approach involves trapping stray and feral cats, having them spayed or neutered, and then returning them to their outdoor colonies where they have adapted to live. TNR helps stabilize cat populations and prevents future litters from being born. Read more about TNR in one of our other blog posts and check out our list of TNR organizations that provide services in the Denver metro area if you’d like to get involved or need support.
Whether or not you can adopt or foster, there are plenty of ways to make a difference! Here are just a few ways you can help:
EduCATion is key to supporting our cat population—it’s built right into the word! Share information about kitten season, TNR programs, and responsible pet ownership with your community. Social media, local events, and word-of-mouth can all help raise awareness and encourage others to get involved.
Follow us on Instagram, Facebook, and TikTok for helpful, shareable content. Sign up for our email newsletter, aka our Mewsletter, to stay updated on upcoming events, adoptable cats, must-read stories, and ways to support the shelter. We also publish a quarterly print newsletter called Cat Care Quarterly that you can sign up to receive at home for free!

Kitten season is a challenging time for shelters and rescues, but with community involvement, we can help save lives and reduce the number of homeless cats and overcrowded shelters. Whether you open your home to a cat in need, contribute supplies or funds, or simply spread the word, your support makes a meaningful impact. CCS is grateful to all of our supporters, including our dedicated volunteers, fosters, donors, adopters and beyond. Let’s continue working together to give kittens the best start in life and create a brighter, more hopeful future for all cats!
About the Author: Beth Dokolasa is a volunteer for Cat Care Society and served on the organization’s junior board. She is an instructional developer for Natural Grocers and lives in Indian Hills, Colo., with her husband, daughter, and two cats, Techno and Digit.





In the realm of feline health, panleukopenia, commonly known as panleuk, has long been a significant health challenge, especially for young kittens and unvaccinated cats. As a highly contagious and often fatal disease, panleuk can rapidly devastate entire cat shelters. Fortunately, here at Cat Care Society (CCS), we have a compassionate and innovative veterinary care team, including Dr. Cecily Palamara, our lead veterinarian. In this post, you’ll get to learn from her expertise, including the causes and symptoms of panleuk, as well as how CCS is giving cats a fighting chance to overcome a disease that traditionally carries a grave prognosis.
Panleuk is the cat counterpart of the parvovirus in dogs, targeting rapidly dividing cells in the gastrointestinal tract. Dr. Palamara emphasizes the destructive nature of the virus, causing massive and often bloody diarrhea, leading to dehydration, lethargy, vomiting, hypothermia (due to loss of fluids), and even sepsis. Notably, it also attacks white blood cells, resulting in leukopenia and a weakened immune system. Early symptoms include lack of appetite, lethargy, vomiting and diarrhea, often with blood. (Fun fact: Leukopenia literally means low white blood cell count.)
Panleuk is a serious condition with a poor prognosis; typically, only 20% of cats with it survive three to five days after diagnosis. At CCS, our survival rate is much higher, thanks in part to our proactive approach and early intervention. More on that soon!
Learn more about panleukopenia in this video from Kitten Lady:
The transmission of panleuk in cats and kittens primarily occurs through fecal-oral contact, where they are exposed to infected feces. Contaminated items such as food, water bowls, toys and bedding can contribute to its spread. Additionally, people may inadvertently carry the disease on their clothing and shoes. Even after a cat is cleared of the virus, they can continue shedding it in their feces for an extended period.
Panleuk is more widespread in summer, due to kitten season, and in wetter months due to how the virus lives in the environment. However, panleuk poses a constant year-round threat as it can survive in most environments for an extended period, up to a year! It is even resistant to certain disinfectants, including alcohol and iodine.
“We have to be really careful about contagion control in the shelter,” said Dr. Palamara. “Because it survives in the environment for so long, it’s so important to be practicing good hygiene and good contagion control for anyone that is coming in. We can all work together to keep our shelter as disease free as possible.”
Prevention is always best; the FVRCP vaccine, included in routine vet and shelter care, is the most effective in providing protection. Early detection has also been key to Cat Care Society’s higher than average survival rate. Dr. Palamara and the medical team at CCS conduct panleuk tests on all kittens under a year, aiding in early detection of mild cases. They also treat all cases aggressively. Because panleuk is so contagious, CCS would need a dedicated ward for panleuk treatment, which is something being considered as a part of future building improvements. Currently, the team aims to move infected cats to one of our experienced fosters for personalized care within 24 hours of diagnosis, minimizing the risk of spreading the illness to other cats.
“In previous shelters that I’ve worked at, even a totally bright alert kitty that’s blowing diarrhea and has panleukopenia gets euthanized on the spot,” said Dr. Palamara. “So [at CCS] it’s a very different approach than I’ve ever worked with, and it’s been a great learning experience for me to see how these guys can succeed.”
Raechel, one of our experienced fosters, has helped treat several CCS kittens with panleuk. She emphasizes that subcutaneous fluids administered once or twice a day, along with antibiotics, anti-nausea medication, heat, nutritional supplements and probiotics, facilitate a kitten’s ability to continue eating and growing during recovery. While there’s no cure for panleuk, this supportive care alleviates the worst symptoms.

“Even in young kittens, symptoms start to improve in just a couple of days with supportive care,” Raechel said. “Before I started panleuk fostering, I heard about how scary and terrible this virus can be, especially for kittens. I’ve found that as long as they’re given these fluids once or twice a day during their worst symptoms, they’ll continue to eat, grow, and bounce back pretty quickly! It’s amazing to see how much better these kittos feel after getting a boost of hydration.”
Raechel, along with all our fosters, has access to CCS’ medical experts for assistance when needed.
Panleuk might be scary, but there are ways to minimize its spread. Here’s how you can be a part of the solution:
Despite its severity, cats can overcome panleuk when it’s found early and treated aggressively. The proactive measures we take at CCS and the dedication of our foster care volunteers showcase the transformative impact of compassionate care. We hope to continue to pave the way for success stories by spreading awareness and support.
For even more information about panleuk, please visit the panleuk shelter medicine page from UC Davis. Learn more about our CCS medical team and all the life-changing work they do on our meet our shelter medical team page.
If you’re interested in becoming a foster to help cats in need, please visit our foster page to learn more and apply!
About the Author: Beth Dokolasa is a volunteer for Cat Care Society and served on the organization’s junior board. She is an instructional developer for Natural Grocers and lives in Indian Hills, Colo., with her husband, young daughter, and two cats, Techno and Digit.

If you’ve ever browsed cat adoption profiles and come across the phrase “feline herpes positive,” you might hesitate at first. It sounds intimidating—but it doesn’t have to be. With a bit of knowledge and some extra loving care, cats with FHV-1 can live happy and healthy lives just like any other cat. In this article, you’ll learn what feline herpes is, what can trigger flare-ups, and how simple, informed care can make adopting an FHV-1 cat a deeply rewarding experience.
Because of its latency and potential reactivation, FHV‑1 is often misinterpreted as a chronic disease—but it behaves more like a “flareable” virus than a constantly debilitating one.
Feline herpesvirus type 1 (FHV‑1), also called feline viral rhinotracheitis (FVR), is one of the most common viral infections in cats. Any cat can contract FHV-1, but younger cats are most often affected. FHV-1 can be spread through saliva as well as nasal and eye discharge, either directly from the cat or from a contaminated object like a toy or food dish. After initial exposure, the virus typically causes an upper respiratory and ocular infection (sneezing, nasal/eye discharge, conjunctivitis) lasting around 10–20 days in mild cases.
Even once the acute symptoms have resolved, the virus remains in a dormant state in nerve tissues for the cat’s life. The virus is most likely to reactivate if the cat experiences stress or an immune system challenge. When it reactivates, it causes a flare-up. Many cats experience very mild or even subclinical symptoms when a flare-up occurs.
FHV-1 vs. FIV vs. FeLV
It’s easy to confuse FHV‑1 with other feline viruses like FIV (feline immunodeficiency virus) or FeLV (feline leukemia virus), but they’re quite different. FHV‑1 is a respiratory virus that causes flare-ups like sneezing and eye discharge, but doesn’t impact a cat’s immune system the way the other two do. FIV is an immune-compromising virus primarily spread through deep bite wounds, while FeLV is a retrovirus that can suppress immune function and is more easily spread through prolonged close contact like grooming or shared dishes. Each virus has its realities, but none are an automatic disqualifier for a loving, quality life.
Myth 1: “Having FHV-1 means the cat will have a low quality of life that’s filled with constant illness and discomfort.”
Reality: Most cats recover from initial infection and go on to lead essentially normal lives. While younger kittens, immunocompromised cats, or those with other illnesses might experience a more severe disease, serious outcomes are relatively rare in otherwise healthy cats.
Myth 2: “A cat with FHV-1 will always be symptomatic.”
Reality: Many cats are asymptomatic carriers most of the time, with flare-ups only under stress (e.g. moving, travel, other illness). In fact, viral shedding (when the cat is contagious) is much more likely during active episodes; in dormancy, shedding is minimal or absent.
Myth 3: “Herpes in cats is like herpes in people and can spread to humans or dogs.”
Reality: FHV‑1 is species-specific; humans and dogs cannot contract feline herpes.
Myth 4: “You can cure FHV-1 completely.”
Reality: There is no cure for herpes in cats. The goal is managing symptoms, reducing flare frequency and severity, and supporting the cat’s overall health through good nutrition and enrichment.
Myth 5: “You can prevent FHV-1 completely.”
Reality: One of the core vaccines recommended for kittens and adult cats by the Feline Veterinary Medical Association is the FHV-1 vaccine. While this vaccine doesn’t completely eliminate the chances of the cat contracting FHV-1, it is highly effective at preventing severe illness, including symptom severity and duration, and it also helps limit the cat’s viral shedding and how contagious it is to other cats. This vaccine is often administered as part of a combination vaccine called FVRCP, which protects against Feline Viral Rhinotracheitis, Calicivirus, and Panleukopenia. All cats at Cat Care Society are given the FVRCP vaccine according to the recommended schedule.
As you can see, the reality is that cats with FHV-1 can still live long, happy lives with proper care, love, and a stable environment that supports their health and comfort.
If a shelter informs you that a cat you’re interested in adopting has FHV-1, keep the following considerations and tips in mind to help your future feline friend thrive:
At CCS, if a cat is suspected of having feline herpes, it will be noted in their medical records along with information about the virus. It’s also important to understand if the cat has any other co-existing conditions, like upper respiratory illness or eye concerns, that might complicate flare management. Understanding the individual cat’s history gives you a more accurate sense of what to expect so you can be prepared. You should also share this information with your veterinarian so they can create a treatment and management plan. In most cases, FHV-1 symptoms are non-life threatening and the cat will respond well to general supportive care.
Be aware of the respiratory and ocular signs of a flare-up, such as sneezing, watery eyes, discharge, and corneal irritation or ulcers, especially in times of stress. During those times, vet support (antivirals, topical ocular medication, secondary infection treatment) plus extra care at home can often resolve symptoms.
Stress is one of the strongest triggers for viral reactivation. Strategies to help minimize stress include:
Even when asymptomatic, certain practices, in addition to stress reduction, can reduce flare risk and flare severity:
Many potential adopters hesitate when they see an FHV-1–positive cat, but choosing to adopt one and offering them a loving home can be truly life-changing—for both of you. Here at CCS, we’ve received many heartwarming updates from adopters whose herpes-positive cats are thriving, underscoring that with care and compassion these cats can live long, joyful lives. If you’d like more information on FHV-1, including details on how the virus works and common treatment regiments, check out this great article by VCA Animal Hospitals.
About the Author: Beth Dokolasa is a volunteer for Cat Care Society and serves on the Board of Directors. She is an instructional developer for Natural Grocers and lives in Indian Hills, Colo., with her husband, daughter, and two cats, Techno and Digit.

When was the last time you took your cat for a wellness exam? If you can’t remember, this article is for you—and you’re definitely not alone. Many people don’t consider taking their cat to the vet unless there’s an obvious issue, but this can unfortunately jeopardize their health and well-being. Cats are experts at hiding pain and illness, and by the time a problem becomes visible, it may already be advanced. Routine veterinary care is one of the most important things you can do to keep a cat healthy throughout their life.
Cats instinctively mask pain or weakness. Problems common for cats, such as kidney disease, dental disease, or thyroid issues, can develop silently for months or even years. Regular wellness exams give veterinarians the chance to catch developing issues before they become more serious, improving long-term health and treatment outcomes.
Wellness exams cover much more than a simple once-over. Vets examine the cat’s teeth, skin, heart, lungs, weight, eyes, joints and internal organs. They also recommend vaccines, blood work, and parasite prevention. Addressing problems early usually means less invasive treatment, lower costs, and smoother recovery.
Wellness checkups are also a great time for you to ask any questions you might have specific to your cat, such as food recommendations, dental care, dietary supplements, or behavioral concerns.
Many people assume indoor cats are safe and need less medical care. While indoor living reduces some risks, it does not eliminate certain diseases or chronic medical issues. Indoor cats commonly struggle with obesity, dental problems, stress-related conditions, and age-related diseases that develop over time. Vets recommend checkups for indoor cats just as consistently as outdoor cats.
Cats often reach their senior years before their owners notice the subtle behavioral changes that come with aging. Because age-related illnesses can progress more quickly in older cats, more frequent checkups help ensure timely diagnosis and better support your cat’s health and comfort. Below are the minimum visit recommendations by the Merck Veterinary Manual based on cat age.
Don’t wait for the next scheduled checkup if you notice any changes in your cat, such as shifts in appetite, grooming habits, litter box behavior or output, energy levels, sneezing, increased scratching, or any other behavioral changes—make an appointment with your veterinarian. Addressing concerns early is not only better for your cat’s health but it can also give you peace of mind.
The CCS website lists a range of veterinary and medical resources for cat owners, including wellness services, low-cost clinics, and emergency care options. If you have pet insurance, review your plan details to see whether you also enrolled in a pet wellness plan, which can help cover routine care expenses. New to pet insurance? Check out our insurance guide for cat owners. All of these resources exist for a reason: cats need medical support just as much as dogs do, they are simply better at hiding it.
About the Author: Beth Dokolasa is a volunteer for Cat Care Society and serves on the Board of Directors. She is an instructional developer for Natural Grocers and lives in Indian Hills, Colo., with her husband, daughter, and two cats, Techno and Digit.

The 2026 Cat Care Society calendar is now available for sale online or in our Meow Mart store in the shelter!
Grab your “Silly Shelter Cats” calendar today featuring silly pictures from our adoptable cats, plus photo updates from some of our amazing alumni!
Shipping is available to all U.S. states for just $5.


There are more cat food options than ever before, which is great for picky eaters and for cats with special dietary needs, but for a cat owner, navigating the cat food aisle can feel overwhelming. The good news is that with so many options available, even if you’re on a budget, you can still provide your cat with healthy and tasty food. In this article, we will discuss what to look for on the label, pros and cons of various cat food forms, and much more!
The best way to begin filtering through all the cat food options is by knowing what to avoid and what to look for on the product’s label.
What to Avoid:
Food Fact: Terms like “premium,” “gourmet,” “holistic,” “no fillers,” and “human-grade” aren’t legally regulated and don’t guarantee higher-quality ingredients. While foods with these labels aren’t always bad choices, it’s important not to rely solely on these words when choosing a cat food, as they have no official definitions or standards.
What to Look For:
If you’re still having trouble making a decision, you can always ask your veterinarian for suggestions. If your cat needs a specific prescription diet, always follow your veterinarian’s guidance. Also, if you’re adopting a cat, ask the shelter what food the cat has been eating and what they’d recommend. At Cat Care Society, we’re a big fan of Hill’s!
Food Fact: The terms “complete” and “balanced” are defined by AAFCO and are regulated by the Food and Drug Administration (FDA). You can feel confident that when you see “complete” on a cat food, it contains all the required nutrients for a cat. “Balanced” means it contains all the nutrients and they are in the ideal proportions.
Below are the most common forms of cat food. There’s no single perfect choice for every cat, so you may need to experiment to find what best suits your cat’s tastes and your lifestyle.
Dry Kibble: Shelf-stable, cost-effective, and convenient to measure and store, dry kibble is often a significant part of a cat’s diet. There are many options available—from formulas with specific textures to help reduce plaque and tartar, to those fortified with vitamins, minerals, and other specialty ingredients aimed at specific health goals.
Canned/wet food: Containing 70–80% moisture, canned/wet food can support kidney and urinary tract health, especially in cats that don’t drink much water. Wet food is usually very popular with cats, and sometimes essential for cats with dental issues. Some kitties may have a preference between pâté, chunks in gravy, flakes, shredded, etc., so try single cans first before buying in bulk!
Fresh/refrigerated food: This option involves fresh, but cooked, foods that are often steamed to preserve nutrients while reducing harmful pathogens. Safe food handling is still essential to ensure the food remains safe to eat throughout storage and consumption, and be sure to look for complete and balanced options.
Raw/freeze-dried raw food: The goal of commercial raw/freeze-dried raw food is to provide high-quality protein and mimic a cat’s natural prey-based diet. However, most raw cat food products are not complete and balanced, and they also carry a much greater risk of foodborne illness in your pet and in the people living in the household. Additionally, it is not recommended to feed your cat raw meat purchased at a traditional grocery store as it carries a greater risk of illness due to harmful bacteria like Salmonella and E. coli. In recent years, feeding cats raw and freeze-dried cat food has also come with an increased risk of bird flu transmission. The Food and Drug Administration (FDA) has some great research and guidance on raw pet food diets.
Many cats enjoy a combination of foods. This could look like mixing dry food in with a wet pâté at meal time or serving them separately, such as wet food in the morning and dry kibble for their evening meal. The most important thing is to choose foods with a nutritional adequacy statement on the label, which confirms they are complete and balanced and meet AAFCO nutrition standards.
One thing is for sure: cats need meat. Cats are obligate carnivores, which means they need to eat meat to stay healthy. In general, cats do best eating a diet with high amounts of protein, moderate amounts of fat, and minimal amounts of carbohydrates. Check out our blog post that goes into more detail on why cats need to eat meat to learn more!
Food Fact: Each cat is unique, and their dietary needs are unique, as well. General recommendations given in our blog or on the food products you purchase may not be the best fit for your cat. We always recommend consulting your veterinarian when deciding on the best types and amount of food to feed your cat daily.
Whatever you call them, choosy cats can make it difficult to find that balance of nutritious, delicious, and budget-friendly. A good place to start is by switching up the consistency and texture, because a cat’s senses are especially sensitive to it. From having a jaw designed for shearing meat and crunching bones to having highly sensitive whiskers and lips, they notice the subtle differences in food shape, size, and feel. For example, certain cats may love shredded wet food in gravy but stick up their noses to chunks in gravy. Below are some ideas to satisfy your feline foodie.
When to Visit a Vet: If you notice a sudden change in your cat’s food preferences, it’s a good idea to visit your veterinarian to rule out any new health conditions or dental issues. Additionally, if you notice your cat excessively scratching, licking, or biting their skin, it may indicate that they have a food allergy.
By paying attention to the label and choosing foods that meet AAFCO standards for your cat’s life stage and health needs, you can ensure your cat gets the nutrition they need. Remember that different forms of cat food—dry kibble, wet/canned, raw/freeze-dried, or fresh/refrigerated—each have their benefits, and many cats thrive on a mix. For picky eaters, experimenting with texture, temperature, and food enhancers can make mealtime more enjoyable.
Donate you extra cat food to CCS! If you have leftover cat food that your cat doesn’t enjoy or food you simply no longer need, consider sharing it with other cats. CCS gladly accepts any non-refrigerated, unexpired cat food or treats—wet or dry, new or partially used (in their original packaging). Simply bring your donations during shelter hours and leave them in the designated donation area in the lobby.
About the Author: Beth Dokolasa is a volunteer for Cat Care Society and serves on the Board of Directors. She is an instructional developer for Natural Grocers and lives in Indian Hills, Colo., with her husband, daughter, and two cats, Techno and Digit.

When Sunny came to Cat Care Society, she was heartbreakingly fragile. This petite brown tabby faced some of the toughest medical challenges we see in cats: advanced kidney disease, severe anemia, constant vomiting, and dangerous weight loss. Each day, her future seemed uncertain.
But even when she was weak, she never stopped showing us her sunny disposition. She purred through exams and headbutted our staff’s hands as if to say, “Don’t give up on me.”
And we didn’t.
Sunny quickly became a staff favorite at Cat Care Society. That’s why we gave her a special distinction: the “Lonely Hearts Club.” This group is reserved for cats who need a little extra help to find their perfect match — older cats, those with longer stays, or cats facing complex medical needs. Sunny ticked every one of these boxes, but we knew she deserved the chance to find a home where she could feel safe and loved.
To continue receiving the daily medications, fluids, lab work, and constant care that keep cats like Sunny alive, we rely on support from donors like you. Every lab test, every dose of medicine, every gentle pat from our veterinary team is only possible because someone chose to give.
Most importantly, generosity from donors like you gave her the greatest gift of all: time. Time to grow stronger, stabilize, and wait for someone who would open their heart to a 14-year-old cat with lifelong medical needs and costly care.
After five months of care in the shelter, Sunny met her perfect match. A local veterinarian met Sunny and instantly knew they were meant to be together. Able to provide the ongoing medical attention Sunny so desperately needed, she was able to give Sunny a loving and restorative home to live out her golden years.
“Sunny (now called Cardi) is doing great! She is a very sweet girl, loves pets and cuddles, and has adjusted well. Her kidney disease is also doing well, her anemia is holding steady, and her weight has continued to go up. I love senior kitties and helping them feel the best they can by managing any medical issues.” – Dr. Hale, Sunny’s adopter

At Cat Care Society, every cat’s care is guided by a compassionate and expert approach — combining veterinary protocols, staff training, donor-funded medical treatments, and specialized initiatives like the Lonely Hearts Club. Sunny’s recovery was not a one-time miracle, but the result of this proven approach designed to identify, treat, and advocate for our most vulnerable feline friends.
Today, Sunny is no longer a lonely heart. She is safe, cherished, and adored — thanks to supporters like you.
But while Sunny’s story has a happy ending, many other Lonely Hearts are still waiting at Cat Care Society. Senior cats. Cats with medical challenges. Cats who have been overlooked time and again. They are counting on us, and on you, to give them love, care, and a second chance at life.
Will you open your heart today to help the next lonely heart find their loving home? Your gift provides the medications, veterinary care, and loving support that make happy endings like Sunny’s possible.
With gratitude,
– EC Michaels

Cats are often known for being picky eaters—whether it’s an aversion to certain kibble shapes, a preference for pâté over chunks in gravy, or a liking for food served slightly warmed. For cat owners, finding a food that their cat enjoys while still meeting nutrition needs can be a real challenge. However, one thing remains certain: cats are obligate carnivores and need to eat meat.
An obligate carnivore is an animal that must eat meat to survive because its body is biologically adapted to derive essential nutrients solely from animal-based sources. Cats evolved as hunters that consume prey containing high amounts of protein, moderate amounts of fat, and minimal amounts of carbohydrates, and they still typically do best consuming those proportions today. Just like humans, cats also require certain amounts of micronutrients, like vitamins, minerals, and amino acids to thrive.
Cats require many kinds of micronutrients from a variety of sources. Below are some of the key nutrients that are either exclusively found in meat or for which meat is the best source.
Without adequate intake of these vital nutrients, cats can experience deficiency symptoms and even irreversible damage to their health, so it’s important to provide them with a complete and balanced diet that reflects their biological need for meat-based nutrition.
Food Allergy Note: Even though cats need meat, they can still develop allergies to certain kinds of meat. The most common meat allergens for cats are beef, chicken, and fish. If you regularly feed these to your cat and notice them scratching, licking, or chewing themselves more than usual, they may have a meat allergy. Your cat’s veterinarian may recommend an elimination diet trial where you avoid the foods they regularly eat for a designated time to see if the symptoms improve. Alternative meat protein like rabbit, duck, and venison are often good options for cats with known meat allergies.
If you’re starting to think this is all leading to a time-consuming recommendation for homemade, all-meat meals—don’t worry. Regardless of quality, feeding your cat only prepared muscle meat (such as chicken breast or ground turkey) can actually lead to essential nutrient deficiencies! Cats need a variety of nutrients found in organ meat and animal fat, too. For balanced and complete nutrition, cats typically do best consuming commercially balanced raw and cooked food.
Look for products that contain a nutritional adequacy statement on the label. This indicates that the food meets the nutritional standards set by the Association of American Feed Control Officials (AAFCO), a nonprofit that establishes nutritional standards for pet foods. Cat Care Society is a proud partner of Hill’s Food, Shelter & Love program, and we feed Hill’s to our shelter cats. Hill’s recipes meet AAFCO nutrition standards, so our cats get the complete and balanced nutrition they need. (Note: AAFCO does not directly test or certify pet foods. Pet food companies use third-party testing agencies to analyze their foods according to AAFCO guidelines.)
Supplemental homemade meals can often be included as a part of your cat’s healthy diet, provided that it’s approved by the cat’s veterinarian, safely prepared, and does not include any ingredients harmful to cats, such as garlic, onions, raw eggs, and excess sodium. Additionally, do not feed your cat raw meat. While cats eat raw meat in the wild, feeding them raw meat purchased at a traditional grocery store can cause illness due to harmful bacteria like Salmonella and E. coli.
Understanding your cat’s biological need for meat is essential to supporting their lifelong health and well-being. As obligate carnivores, cats rely on meat not just for protein, but for critical nutrients like taurine, arachidonic acid, and essential vitamins that they cannot make on their own. By choosing high-quality commercial foods that meet AAFCO standards and consulting with your veterinarian, you can feel confident that you’re giving your cat the nourishment they need to thrive.
About the Author: Beth Dokolasa is a volunteer for Cat Care Society and serves on the Board of Directors. She is an instructional developer for Natural Grocers and lives in Indian Hills, Colo., with her husband, daughter, and two cats, Techno and Digit.

Cat Care Society is proud to announce 29 local artists selected for the 2025 “Tails of the Painted Cats” (TOPC) exhibition. These Colorado creatives have each transformed fiberglass animal sculptures into stunning, one-of-a-kind works of art, now on public display and set to be auctioned this fall to benefit the shelter’s life-saving programs.
Now in its tenth year, Tails of the Painted Cats has become CCS’s signature fundraiser and a beloved event in the Denver arts community. The event brings together artists, animal lovers, and supporters to celebrate compassion through creativity.
“What began as a small, unique fundraiser has grown into a cherished tradition,” said Cat Care Society Executive Director EC Michaels. “As our largest fundraising event, every ticket, bid, and vote truly makes a difference, supporting critical medical care, enrichment, and safe housing for the more than 1,000 cats who come through our shelter each year.”
Seventy-five artists applied for this year’s collection, of which 29 were selected to create animal sculptures. The sculptures are currently on tour.
This year’s exhibition includes:
|
|
“It’s been an incredible joy to watch this event grow over the years,” said Jane Dorsey, Cat Care Society’s longtime Art Director. “This year’s collection is one of our best yet—full of creativity, love, and spirit.”
Tara Deenihan, Art Coordinator and incoming lead for the program, added: “The artists participating this year have truly blown our minds! We have several new artists and many returning artists, and seeing their ideas come to fruition has been really exciting. The cats are all so different and beautifully realized – I love seeing what cats can inspire.”
The public is invited to view the sculptures in person or online and vote for their favorite in the People’s Choice Award. The winner will be announced at the TOPC gala on October 18, and the artist will receive a cash prize.
This year’s TOPC gala will take place Saturday, October 18, 2025 at Pinehurst Country Club and will be masquerade themed. 9News Reporter, Steve Staeger returns as this year’s emcee. Tickets will go on sale in mid-June.
Learn more about Tails of the Painted Cats at catcaresociety.org/topc/

At Cat Care Society, we know that caring for cats is a team effort—and one of the most important parts of that team is our foster network. While our shelter provides safe, dependable housing and veterinary care for hundreds of cats each year, foster homes offer something we can’t always replicate within our walls: a quiet, individualized space where certain cats can truly thrive.
Foster homes complement the work shelters do. They enable us to have a flexible and responsive system that helps more cats heal and grow, and they allow us to stretch our resources further, provide individualized support to vulnerable cats, and ultimately increase each cat’s chances of getting adopted.
Below are just a few of the ways that foster homes support shelters and countless cats, both directly and indirectly!
Shelters provide a lifesaving refuge for cats, offering medical care, nutrition, protection, and enrichment. But for certain cats, especially those with special needs, a home environment can offer extra support that helps them recover, adjust, or grow in ways that a busy shelter environment might not allow.
Foster care can be beneficial for:
These cats benefit from one-on-one attention and a stable environment where they can relax and show their true personalities.
Foster care expands a shelter’s capacity. Every cat that goes into a foster home opens up space in the shelter for another animal in need. This is a critical part of how shelters operate, especially during busy seasons when intake numbers rise.
Fosters also allow shelters to:
Foster care is not a separate system—it’s part of CCS’ toolkit, allowing us to stretch our impact and offer flexible, creative solutions when cats need them most.
Cats in foster care often show their true personalities more readily than they might in a shelter. This helps CCS provide more information to potential adopters get a clearer sense of whether a cat is the right fit for their home.
Foster homes play a critical role in:
The result? Cats who are more confident, better understood, and great candidates for adoption!
Strawberry (shown at the top of this post) came to CCS as an extremely fearful cat who demonstrated this fear with aggression. We’re talking about spitting, hissing, growling, and lunging at CCS staff, completely unprovoked. A medical workup ruled out any underlying medical conditions that could be contributing to the behavior. Strawberry was a great candidate for a quiet foster home where she could have space, get comfortable, and work on socialization at her own pace.
In just over a week, a report from the foster stated that Strawberry had become a lap cat, was accepting and demanding pets, and had begun giving “head boops” or bunting, which is one way cats show affection. The foster was also able to quickly pick up on Strawberry’s motivations, favorite toys, and preferred ways to receive pets which accelerated Strawberry’s comfort level and ability to socialize. With patience and gentle care, Strawberry came out of her shell and built a lot of confidence.
After just under two months in the foster home, Strawberry came back to the shelter and was adopted a short time later!
At Cat Care Society, we’re proud to offer a safe, well-equipped shelter environment for our cats. But we also recognize that cats, like people, have individual needs. Foster homes allow us to meet those needs with compassion and flexibility.
Foster homes don’t replace shelters—they enhance them. Together, we’re able to give each cat the kind of care that works best for them. Whether it’s a cat recovering from surgery, a shy kitten learning to trust, or a beloved pet temporarily staying with us while their owner gets back on their feet—foster care gives us options. And options save lives and produce the best possible outcomes.
We’re incredibly grateful for our foster caregivers and the role they play in this mission. Because of them—and in partnership with our shelter—we’re able to do more, reach farther, and help every cat get one step closer to home.
Foster homes are the quiet heroes of the cat rescue world. They don’t just provide temporary shelter—they provide special cats opportunities to heal, grow, and shine. Their impact can’t be overstated: they help shelters run more effectively, improve outcomes for individual cats, and create a more compassionate, responsive animal welfare system.
At Cat Care Society, we are deeply grateful for every person who opens their home to a cat in need. If you’re interested in becoming a foster, please apply! We’re especially looking for fosters willing to take in cats with medical needs, those needing behavioral support, mother cats with litters, and young kittens. CCS provides all necessary training and support, including costs for your foster cat’s needs from food to medical care.
About the Author: Beth Dokolasa is a volunteer for Cat Care Society and serves on the Board of Directors. She is an instructional developer for Natural Grocers and lives in Indian Hills, Colo., with her husband, daughter, and two cats, Techno and Digit.

When I walk into Cat Care Society, or any shelter, with my camera, I don’t see homeless pets – I see stories waiting to be told.
I see cats with beautiful personalities just waiting to come out once they find the right person. Some are shy and mysterious, others sassy or playful, but they all have one thing in common: they deserve to find that Right Person. We live in a world where adoptions begin with a scroll on a screen, where the very first impression is what makes a connection, where love at first sight is very real.
That’s where photography comes in. They need not just any photo, but one that speaks err …MEOWS.
Online pet profiles are now often the first step to adoption. A great photo can stop someone mid-scroll, make a potential adopter feel something, and highlight a pet’s unique spirit with their eyes, their head tilt, and their expressive tail.
Think about it this way – would a blurry photo of a dark shadow stop your eyes from scrolling? Or would you instead pause on a well-lit portrait of a clear-eyed feline looking through the phone directly into your soul?
Images like these invite a second look. And that second look can turn into love.

By the time I get to them, most of these cats have had enough days to settle into their new surroundings. Their original intake photo is usually taken just as they arrive. They’re not sure where they are or who these strange people are and it shows. After a few days, most have realized they’re safe. They’ve gotten some sleep, maybe some treatment, delicious food, they generally feel better, and that also shows.
Cleo, as you can see from the intake photo versus the portrait, was all about asking me for attention when I came in to photograph her. Her royal line was becoming obvious! And since then, she has been adopted into a loving family.
While I love volunteering my professional photography for Cat Care Society and others, I know many fosters are doing amazing work on their own — and you want your foster cats to stand out, too.
The next time you see an adoption profile, take a second to really see the cat. If you feel drawn in by the photo – even if just for a moment – know that was no accident.
It was love, caught in a frame.
Susie Inverso owns Crimson Cat Studios Pet Photography in Lakewood, CO. She specializes in capturing the true spirit of companion animals through compassionate, story-driven portraits. You can learn more about her at www.crimsoncatstudios.com




Please include your full name on a gift note when sending donations through Amazon or Chewy, so we can properly acknowledge your generous contribution! Without it, we won’t be able to identify that the items are from you. Also, please keep your shopping receipt, as it serves as your official donation receipt.
Spark a chain of giving! Help us reach our goal today to raise $180,000 for Colorado cats in need!
Double your impact by joining the Cat-alyst Club, our community of monthly donors, and Colorado Gives Foundation will match your first month’s donation!
Place your bids in our silent auction featuring cat-themed sculptures, paintings, pottery, and more!
Bidding will close Saturday, October 18, at approximately 7:30 PM.
The shelter will be closed Thursday, December 25 in celebration of the holiday season.
The shelter will reopen with normal hours on Friday, December 26.
Upcoming events, special announcements, and cute cat photos delivered to your inbox bi-weekly!